Human metapneumovirus (HMPV) is often compared to the common cold due to its mild symptoms in most cases, but it isn’t “just a cold.” It can cause significant respiratory issues, particularly in vulnerable groups such as young children, older adults, and individuals with compromised immune systems or underlying respiratory conditions. While most infections result in upper respiratory symptoms, HMPV has the potential to cause severe lower respiratory infections, such as pneumonia or exacerbations of asthma and COPD.
HMPV (Human Metapneumovirus) and coronavirus (including SARS-CoV-2, the virus that causes COVID-19) are different viruses, though both can cause respiratory illnesses.
Virus Family and Structure
HMPV: Belongs to the Paramyxoviridae family.
It is an RNA virus similar to RSV (Respiratory Syncytial Virus) and parainfluenza viruses.
Primarily affects the upper and lower respiratory tract.
Coronavirus (SARS-CoV-2): Belongs to the Coronaviridae family.
It is an RNA virus with a distinctive spike protein on its surface.
Includes various strains, such as those causing mild colds (e.g., OC43) and severe illnesses (e.g., SARS, MERS, COVID-19).
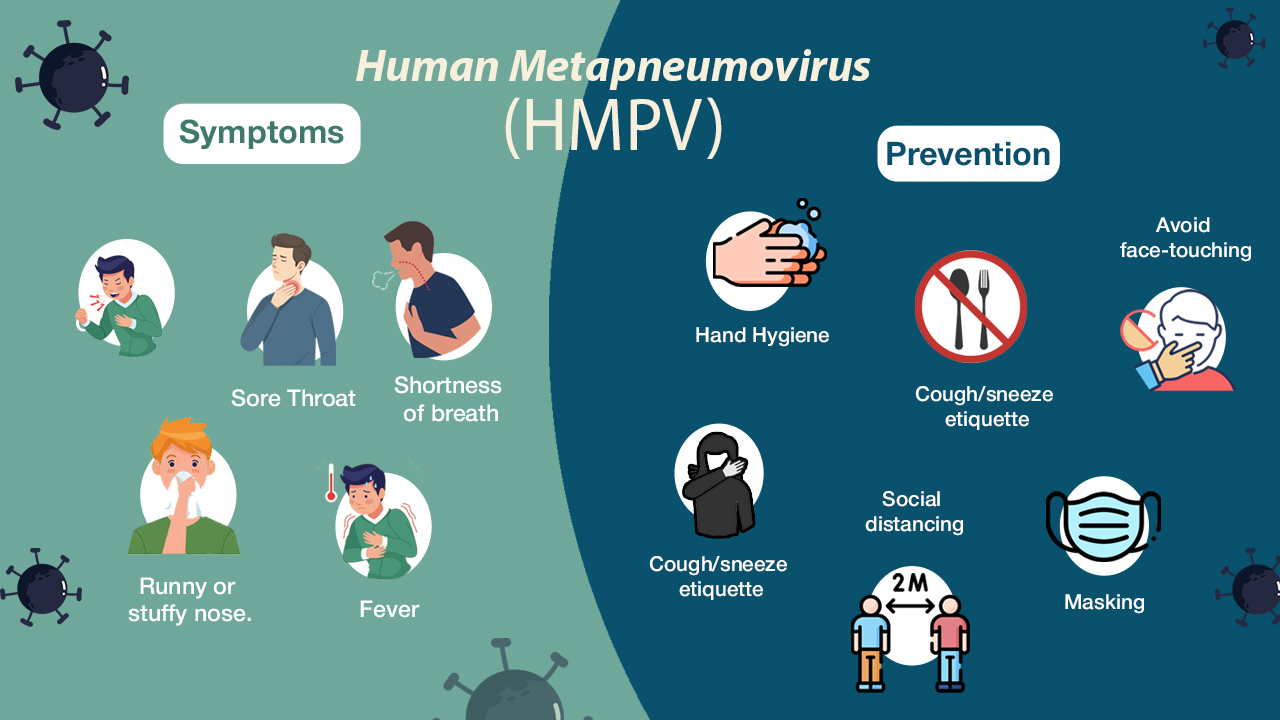
Symptoms
Both viruses can cause respiratory symptoms, but the severity and common symptoms vary:
HMPV: Mild symptoms: Runny nose, cough, fever, sore throat, nasal congestion.
Severe cases: Bronchiolitis, pneumonia, or wheezing (especially in children and older adults).
COVID-19 (SARS-CoV-2): Mild symptoms: Fever, cough, fatigue, sore throat, body aches.
Severe cases: Difficulty breathing, pneumonia, blood clots, organ failure.
Unique symptoms of COVID-19 include loss of taste or smell (in some cases).
Transmission
HMPV: Spreads via respiratory droplets, direct contact with infected individuals, or contaminated surfaces.
Seasonal, with infections peaking in winter and spring.
SARS-CoV-2 (COVID-19): Spreads through respiratory droplets, aerosols, and contaminated surfaces.
Can spread asymptomatically and more easily than HMPV.
Not as strongly seasonal but influenced by population immunity and public health measures.
Severity
HMPV: Typically milder, especially in healthy individuals.
High-risk groups (young children, elderly, and immunocompromised) can develop severe illness requiring hospitalization.
SARS-CoV-2 (COVID-19): Can cause severe disease in all age groups, especially the elderly and those with underlying conditions. Associated with complications like blood clots, long COVID, and systemic inflammation.
Treatment
HMPV: No specific antiviral treatment; symptoms are managed with rest, hydration, and supportive care.
Severe cases may require oxygen or hospitalization.
SARS-CoV-2 (COVID-19): Antiviral treatments like Paxlovid or Remdesivir are available for severe cases.
Vaccines are widely available to prevent severe disease.
Prevention
HMPV: No vaccine yet.
Prevention relies on hygiene practices: handwashing, avoiding contact with infected individuals, and disinfecting surfaces.
SARS-CoV-2 (COVID-19): Vaccines are available and highly effective at reducing severe illness.
Preventive measures include mask-wearing, social distancing, and hygiene practices.
You will observe that the prevention for both these viruses are
- Hand hygiene: Wash your hands with soap and water regularly. If soap and water aren’t available, use an alcohol-based hand sanitizer.
- Cough/sneeze etiquette: Cover your nose and mouth with your elbow when you sneeze or cough.
- Social distancing: Stay away from others when you or they are sick with a contagious illness.
- Masking: Wear a mask if you’re sick and need to be around others.
- Avoid face-touching: Refrain from touching your face, especially your eyes, nose, and mouth.
- Food and utensil sharing: Don’t share food, utensils, or drinks with others.
Vinod Ram has been in Software Industry since 2006 and has experience of over 16 years in Software Development & Project Management domain specialised majorly in LAMP stack & Open Source Technology, building enterprise level Web based Application, Large Database driven and huge traffic Websites and Project Management.
He loves to write information articles and blog to share his knowledge and experience with the outside world and help people to find solution for their problems.